Chronic Wounds of the Legs and Feet
Chronic Wounds
Author: Asad R Shamma, MD, FACS, Vascular Surgeon; SHAMMA Clinic, Dubai, UAE
What is a Chronic Wound (AKA Non-Healing Wound)?
A Chronic Wound is a skin (or barrier) defect that has not healed in 3 months.
Chronic Wounds place a massive burden on patients, their families and on the healthcare system of society. They require intensive care and often result in home confinement and loss of work. Furthermore, they are a financial burden on the patient and the healthcare system: an estimated 5% of the yearly healthcare budget in Western countries is spent on Chronic Wound care and treatment.
Types of Chronic Wounds
There are 3 major types of Chronic Wounds:
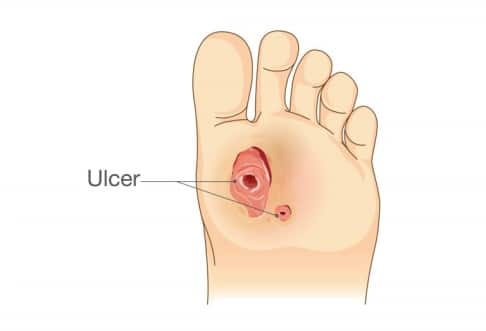
Fig 3: Diabetic Foot Wound (DFW) / Neurotrophic metatarsal Wounds
3. Decubitus Ulcer (DU)*, which mostly occur on pressure areas of the body in immobilized patients (Fig 5)
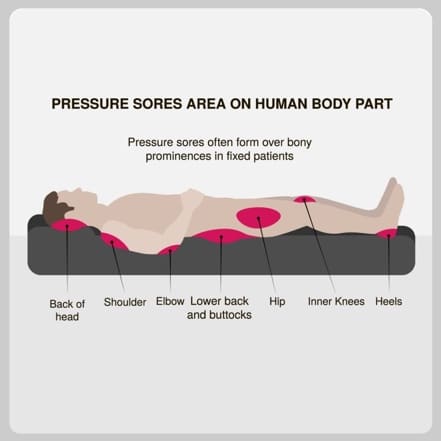
Fig 5: Areas prone to decubitus ulcers
* This article is written in layman’s terms and will concentrate on VLU & DFW. DU will be covered at a later stage.
In this Article
.
- Etiology (Causes)
- Pathophysiology (Mechanism and reason for development)
- Pathophysiology Image Gallery
- Diagnosis
- Treatment
- Prevention
- Case Studies
- Glossary
Article Highlights
The section covering the Pathophysiology of Chronic Wounds will be detailed, to give the reader a better understanding of how to recognize the signs and symptoms of a VLU and a DFW so you seek early treatment for yourself or for your loved one. It will also make the treatment of Chronic Wounds easier to understand. More importantly, you will be able to fully understand and practice the measures of preventing Chronic Wounds from developing.
.
Towards the end of this article is a PowerPoint Presentation (PPT) with real-life examples and case studies of patients with Chronic Wounds treated at SHAMMA Clinic in Dubai. I had the privilege of treating these patients recently. You will see pictures of their Chronic Wounds at different stages of healing – starting from when I first met the patient, until complete healing. This will be followed by 2 interactive video interviews: One video dedicated to DFWs, and another covers VLUs.
.
At the end of the article is a glossary of the specialized and medical terms and acronyms used throughout this article (most of the underlined words and phrases that appear in this article).
I. Etiology (Causes)
The most common etiology of Chronic Wounds on the legs and feet are:
- Peripheral Arterial Disease (PAD): PAD (Fig 6) is a manifestation of atherosclerosis (hardening of arteries). PAD is caused by cholesterol plaque buildup leading to blockages or narrowing in the arteries and resulting in decreased blood flow to the affected leg and foot.
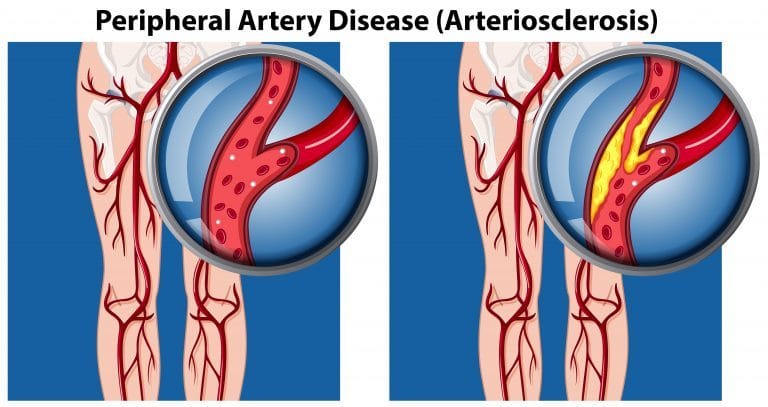
Fig 6: Peripheral Arterial Disease (PAD)
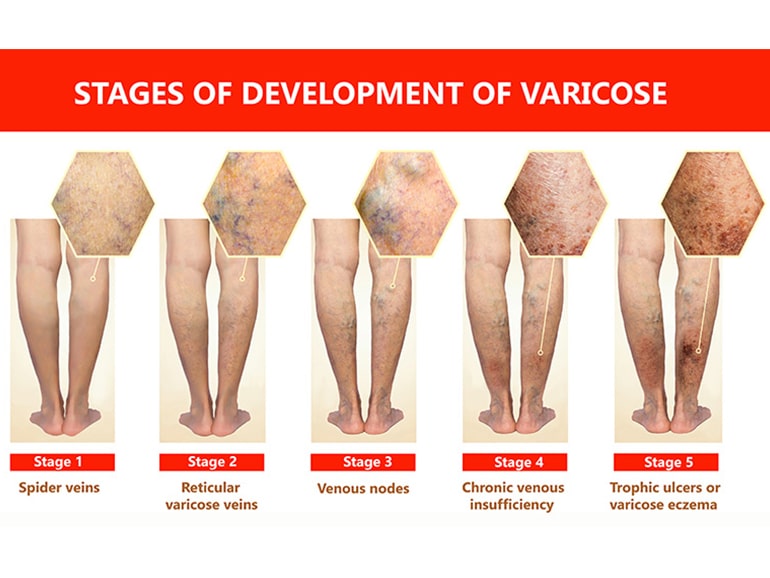
- Venous Insufficiency (VI): This can be caused by Venous Reflux (Fig 12, 13) in patients with Varicose Veins (VV) (Fig 7), combination of obstruction to venous flow return and Venous Reflux as a sequela of Deep Vein Thrombosis (DVT) – (Fig 8). Worthwhile to mention that the constellation of signs and symptoms post DVT are often referred to as Post Thrombotic Syndrome.
 |
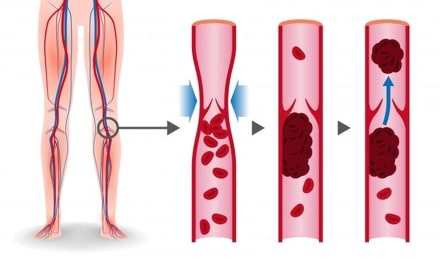 |
Fig 7: Varicose Veins (VV) |
Fig 8: Deep Venous Thrombosis (DVT) |
- Neuropathy: (Fig 9) This is damage to the nerves of the legs and feet, caused by years of poorly controlled Diabetes Mellitus (DM). It is often referred to as Peripheral Neuropathy.
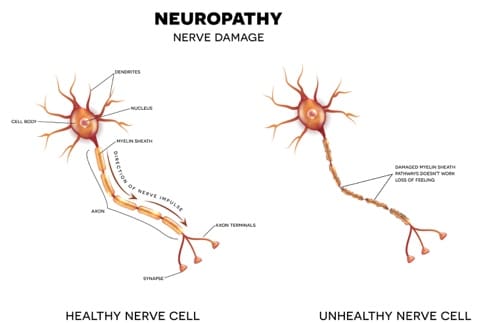
Fig 9: Neuropathy
- Combination of PAD & Neuropathy: In many cases of Diabetes Mellitus (DM), PADand Neuropathy coexist.
II. Pathophysiology
.
- PAD: In this case, the reason for a wound not to heal is the lack of sufficient oxygenated blood reaching the area of the Wound. Wounds need healthy blood carrying oxygen and nutrients to heal. Patients with PAD have blockages in the arteries of their legs, which does not allow sufficient blood to reach the Wound.
- VI (Venous Insufficiency): In VI (Fig 15, 16), venous pressure in the leg veins is high (Venous Hypertension) – (Fig 11) due to either Venous Reflux (Fig 13) or restriction of venous blood return, due to obstruction. When it comes to patients with VI, the blood flow in leg veins is bidirectional (Fig 12, 13) and unoxygenated nutrient-deprived blood pools, which stagnates in dilated unhealthy leg veins and foot veins as patients are standing or sitting; and the blood flow does not return properly and efficiently to the heart. This causes swelling of the feet and legs (Fig 14).
.
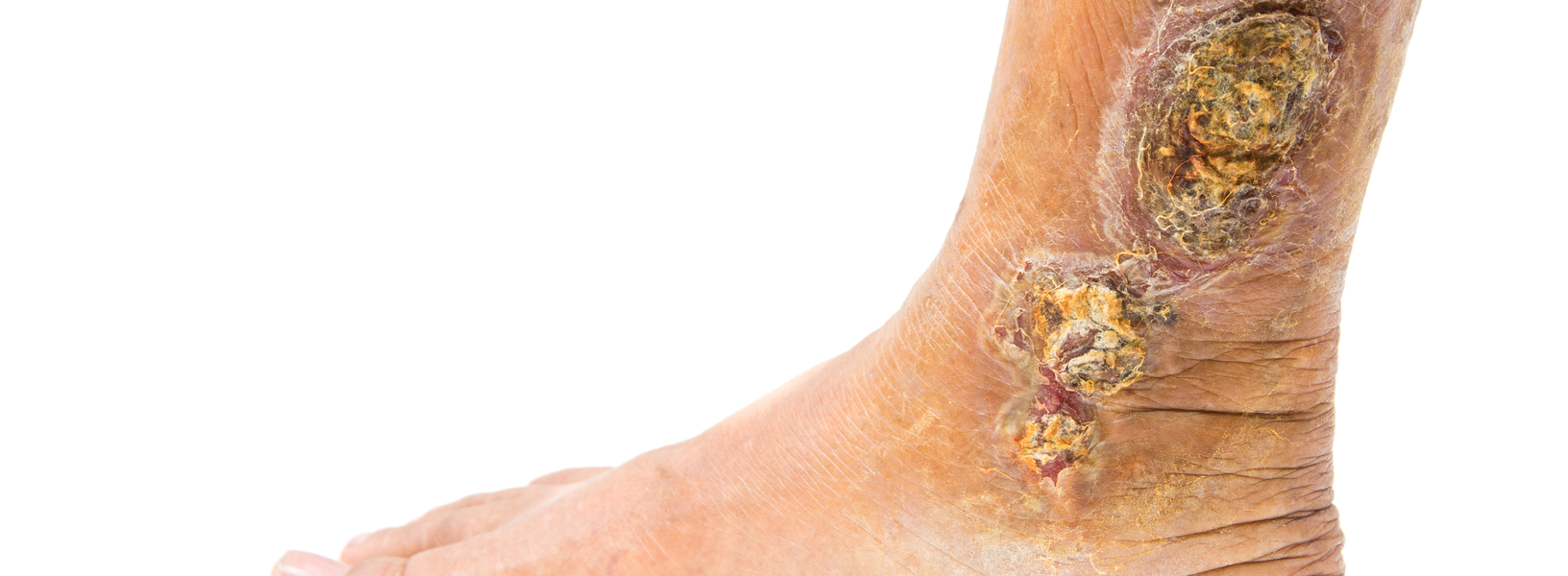
In patients with VI, the skin around their ankles loses its elasticity, and signs of Lipodermatosclerosis and Venous Stasis develop. The skin becomes inelastic, hard, brittle, inflamed, and itchy (Fig 15, 16). Instead of expanding to accommodate the swelling, the skin cracks and ulcerates when the leg swells – resulting in a Wound (Fig 17, 18).
- DM (Diabetes Mellitus / Diabetic Foot): In diabetics, the cause of Chronic Wounds is multifactorial: –
-
- Patients with DM often have PAD in addition to microangiopathy (impairment of blood flood in the small vessels of the feet and legs), so the same factors mentioned under PAD are in play here.
. - Neuropathy: Prolonged DM – especially in patients with poor control of their blood sugar results in damage to the Motor Nerves (nerves that control muscle movement) and Sensory Nerves (nerves that control sensation).
- Patients with DM often have PAD in addition to microangiopathy (impairment of blood flood in the small vessels of the feet and legs), so the same factors mentioned under PAD are in play here.
-

Fig 10: Neurotrophic Metatarsal Wounds – Early Diabetic Foot Wound (DFW)
Malfunction of these nerves results in what is referred to as Chronic Wounds, typically on the sole of the feet, and are referred to as Neurotrophic Wounds (Fig 3, 10).
.
The best way to explain the Pathophysiology of the Neurotrophic Wound is to give you real-life examples:
-
-
-
- When you buy a pair of shoes and wear them excessively immediately, the shoes may put too much pressure on the back of your heels or on one of the prominent bony areas of your toes, which causes pain.
.
In a healthy, non-diabetic patient with normal sensation, he or she will be alerted due to the pain they feel; and will usually take off the shoes or adjust them.
.
In contrast, a patient with DM, who has impaired sensation, will not feel the pain, and will continue to wear the shoes and end up with a blister that leads to an open Wound (Fig 19); as well as an infection without feeling or realizing something is wrong with their foot (because the nerves that give the sensation of pain are impaired).
. - A similar scenario occurs when a patient’s foot is exposed to, for example, hot water (such as when soaking their feet) or heat (sitting next to a heater in the winter).
.
Due to impaired feelings caused by damage to the Sensory Nerves, the water or hot surface can burn their skin, resulting in a Wound without them realizing.
. - This 3rd example illustrates how the motor Neuropathy (damage to the nerves that control the fine muscles of the feet) leads to the development of a type of DFW often referred to as Metatarsal Wound (or Metatarsal Neurotrophic Wound or Pressure Wound) and often appear on the Ball of the Foot (Fig 24).
.
In a healthy person, the Motor Nerves delicately control tens of muscles we have in our foot. So, while a healthy person is walking, their weight is equally distributed on the entire sole of the foot i.e. the whole sole of the foot is in contact with the floor.
.
In contrast, patients with Diabetic Neuropathy, this delicate balancing act does not exist, and the pressure is unequally redistributed to small areas of the sole of the foot which become subject to undue excessive pressure (Fig 20). So, pressure points develop, typically over the heads of one of the Metatarsal Bones (AKA “Ball of the Foot”) – (Fig 24).
.
Initially, this results in the formation of a callus over that area (Fig 21); which eventually breaks down, and leads to a Wound developing (Fig 3). Again, due to impaired sensations, the patient with Diabetic Neuropathy realizes this too late, and a Chronic Wound develops – whereby the healing is slow or made impossible due to the poor circulation and constant pressure applied on that area. This destroys the skin tissue every time the body mechanisms try to heal the Wound.
- When you buy a pair of shoes and wear them excessively immediately, the shoes may put too much pressure on the back of your heels or on one of the prominent bony areas of your toes, which causes pain.
-
-
III. Pathophysiology – Image Gallery
.
|
Fig 11: Progressive nature of Varicose Vein Disease |
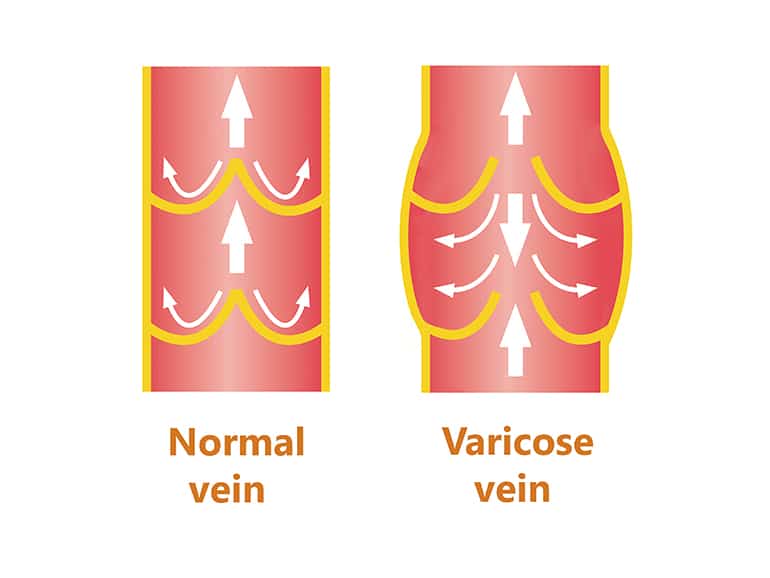
Fig 12: Varicose Vein |
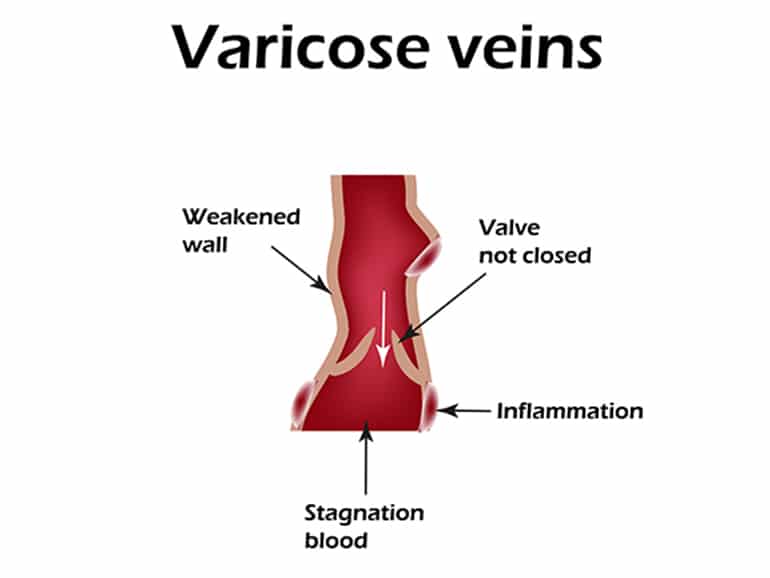
Fig 13: What happens in a Varicose Vein |
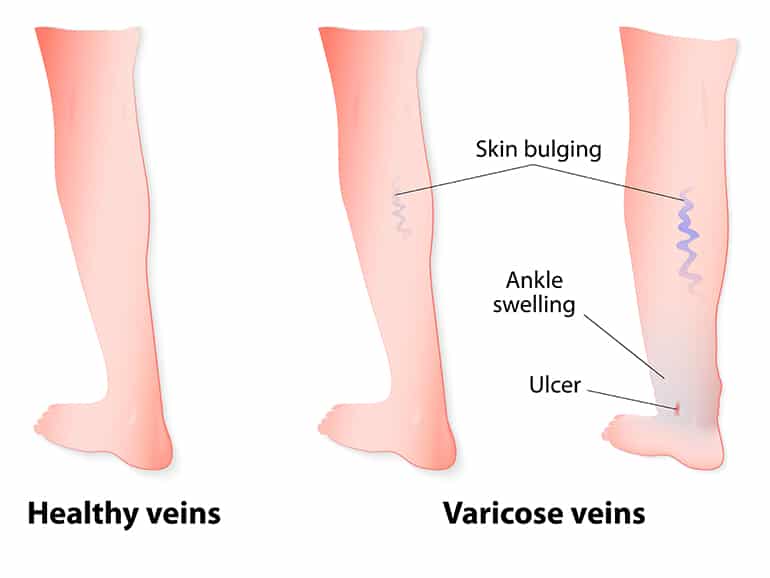
Fig 14: Consequences of Varicose Veins |
|
Fig 15: The spectrum of skin changes in Venous
|
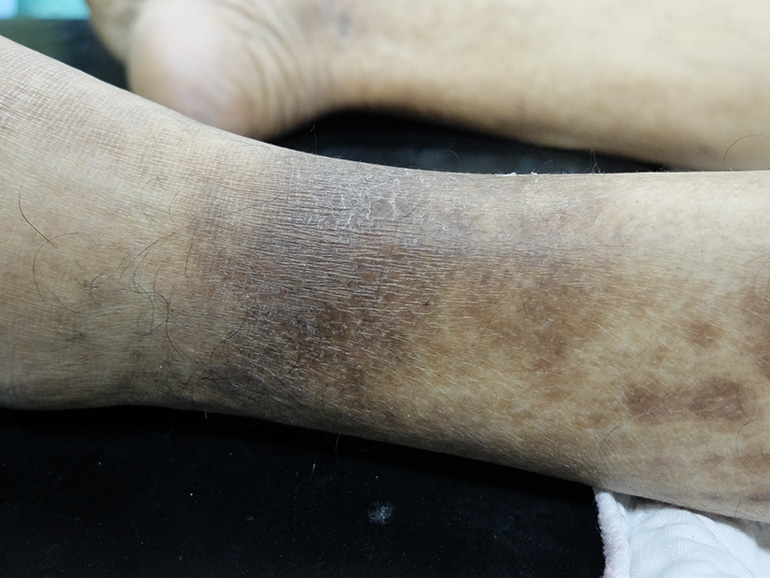
Fig 16: Brittle leathery brown skin in patient with Venous Insufficiency |
|
Fig 17: Early Venous Leg Ulcer (VLU) in a patient with lipodermatosclerosis |
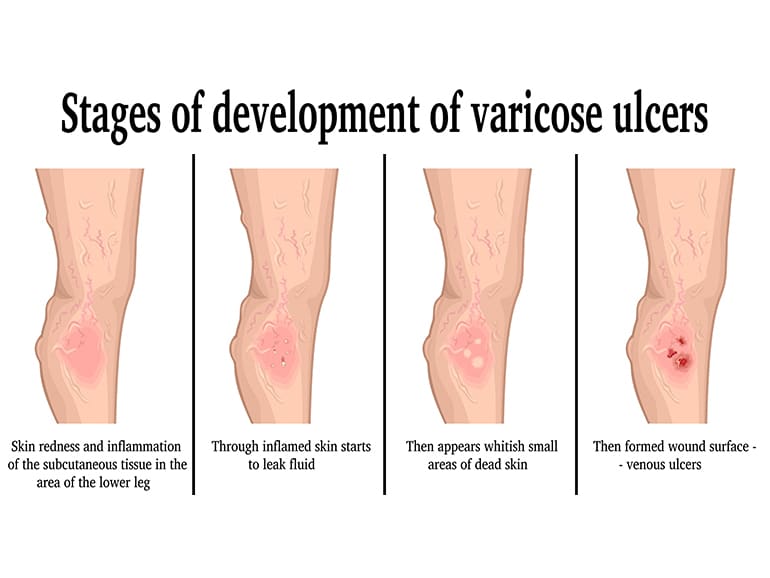
Fig 18: Stages of development of VLU |
|
Fig 19: Heel Blister
|
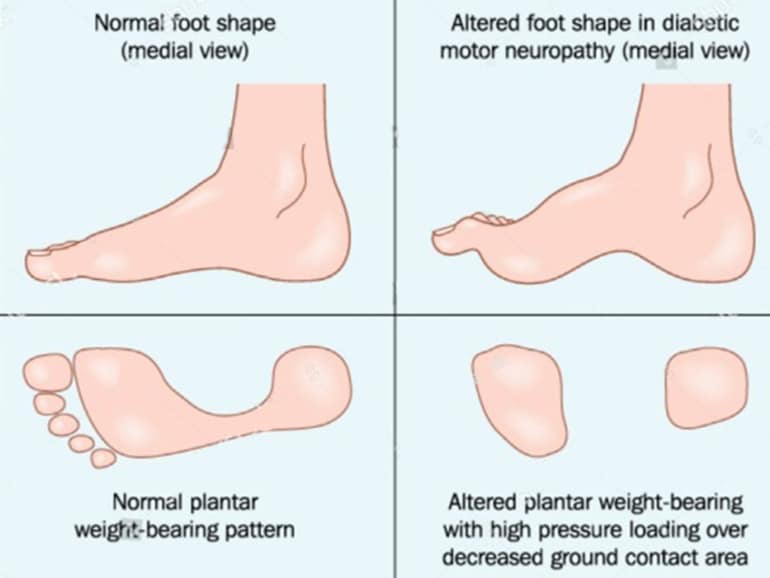
Fig 20: Abnormal weight distribution of weight on sole foot in a diabetic foot |
|
Fig 21: Callus formation over pressure point |
.
IV. Diagnosis
.
The diagnosis of a VLU and DFW is easy and straightforward for an experienced clinician. It starts with your physician obtaining a medical history and the chronology and circumstances of how the Wound developed are extremely essential to your physician.

Fig 22: Duplex Ultrasound Exam of the Legs (Arterial & Venous)
In all cases of Chronic Wounds, the physician will first assess if there is PAD. This is a crucial first step. By examining the arterial pulse on specific areas of the foot by palpation (similar to palpating the pulse on the wrist), the physician can develop a fairly accurate idea about how healthy arterial flow to the leg and foot is. When in doubt or to quantify the severity of the PAD, your doctor will conduct one or two simple, non-invasive diagnostic tests:
- ABI (Ankle Brachial Index)
- Arterial Duplex Ultrasound of the Legs (Fig 22), often mistakenly referred to as “Doppler Test”
These tests will determine if you have PAD in which case your doctor will refer you to a Vascular Surgeon for further evaluation and treatment.
If PAD is excluded, and the arterial blood supply to the leg and foot is deemed to be adequate, the diagnosis and actual treatment of a VLU or a DFW become easy and straightforward:
- VLU: Typically, a VLU occurs in what is commonly referred to as the “Gaiter Area” of the leg. This is the area above and near (Fig 1,2) to the Lateral Malleolus and Medial Malleolus (which are the bony prominences on each side of the ankle).
.
Another tipping point that one is dealing with a VLU is the presence of signs of VI (Venous Insufficiency) which are:-
- Presence of VV (Varicose Veins) – (Fig 7, 14)
- Skin changes referred to as Lipodermatosclerosis and Venous Stasis (Fig 15, 16)
- Leg swelling
- History of DVT (Deep Venous Thrombosis) and signs and symptoms of Post Thrombotic Syndrome
-
When a VLU is suspected or diagnosed, your physician will conduct a Venous Duplex Ultrasound of the Legs (often mistakenly referred to as “Doppler Test”) – (Fig 22) to confirm the diagnosis and determine the exact etiology – vein(s) that have malfunctioning valves and Venous Reflux (Fig 12, 13) or areas of obstruction to venous blood flow – so that they properly addressed and treated – in addition to attending to the Wound itself.
- DFW: A typical DFW occurs in an area on the sole of the foot that is subjected to excessive pressure out of proportion to the rest of the sole of the foot, most commonly the area of the Metatarsal Heads (Fig 23) and the Ball of the Foot (Fig 24). The Wound is usually surrounded by a callus of varying size and thickness, and the patient has a significantly lower (or in most cases complete absence) of sensation in that area.
|
Fig 23: Metatarsal head |

Fig 24: Ball of the Foot |
.
Other less common areas for DFW are over the Lateral Malleolus and Medial Malleolus which are the bony prominences on each side of the ankle (as opposed to VLU which occur above these bony prominences.
.
In DFW the wound is usually exactly over the most prominent area of the malleolus – recall that A VLU typically is above and near the malleolus). DFWs also develop in the area of the heel and over the Achilles tendon. The presence of a wound in any of these areas (malleolus, heel, or Achilles tendon area) is usually a tipping sign to the physician that the patient has PAD.
V. Treatment
- VLU: The most important component for treating a VLU is Compression Bandaging, which should be of the short-stretch or inelastic type (Fig 25)

Fig 25: Application of a short-stretch bandage
Also known as short-stretch bandages, Compression Bandaging is a tubular bandage made of low elasticity material (often cotton) and applied from foot to knee. It significantly reduces leg swelling without the constriction or the “tourniquet effect” which would otherwise hinder the normal flow of body fluids. My preference is for a multilayer Compression Bandaging where the first layer is medicated with Zinc Oxide and Calamin (UNNA Boot).
.
While treating VLU, your physician may also perform one or more of the following:
- Obtain a swab culture of the wound to determine if there is an infection, and the best antibiotic to use if there is one
- Perform Wound Debridemente. cleaning the dead tissue (Fig 26)
- Perform Sclerotherapy(Fig 27) on the Varicose Vein(s) feeding the VLU
- Apply the appropriate Wound dressing
|
Fig 26: Wound Debridement |
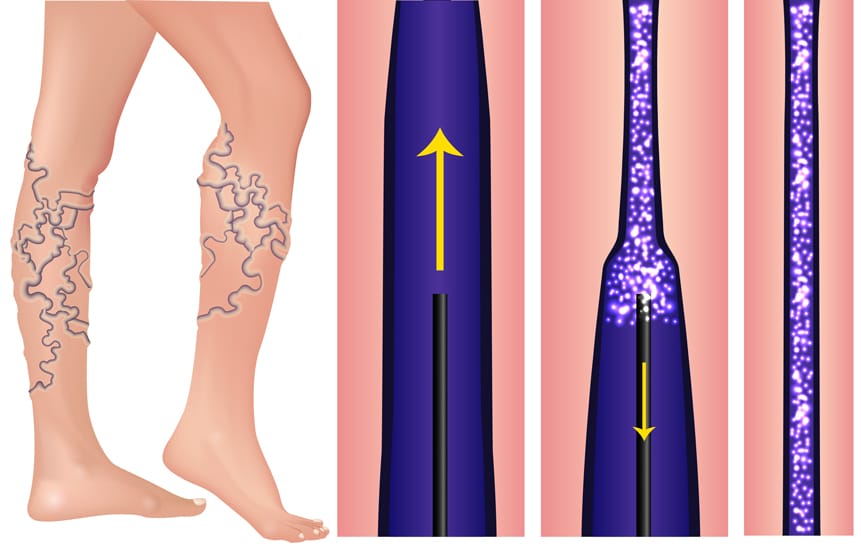
Fig 27: Sclerotherapy of Varicose Veins |
.
Although commonly practiced, there is rarely the need for hospitalization, use of intravenous antibiotics, expensive ointments, or the ever-increasing variety of expensive bandages when it comes to treating VLUs!
- DFW: The most important component for treating a DFW is Offloading (see Fig 28, 29), which is the use of specific types of temporary shoes during the treatment phase of the wound, that takes the pressure of the Wound area (be it a Metatarsal Wound or a Heel Wound).
|
Fig 28: Metatarsal Offloading shoe |

Fig 29: Heel Offloading shoe |
.
- In addition, your physician may perform one or more for the following:
.- Obtain a swab culture of the Wound to determine if there is an infection, and the best antibiotic to use if there is one
- Perform Wound Debridement(i.e. cleaning the dead tissue), which in the case of DFW is the overgrown thick callus tissue that surrounds the wound and impinge on it, thus preventing its healing
- Apply the appropriate Wound dressing
In DFW cases with severe infection, hospitalization and intravenous antibiotics may be needed. Furthermore, it is essential that PAD is excluded or treated by a vascular surgeon concurrent with Offloading and proper Wound care.
.
Using the above treatment plans, we have been able to heal Chronic Wound (VLUs & DFWs) that patients have had for months and sometimes years (see Case Studies included in PowerPoint Presentation (PPT) and Video below) in a matter of few weeks in most cases.
VI. Prevention
- VLU: The following are the recommended preventative measures against developing a VLU.
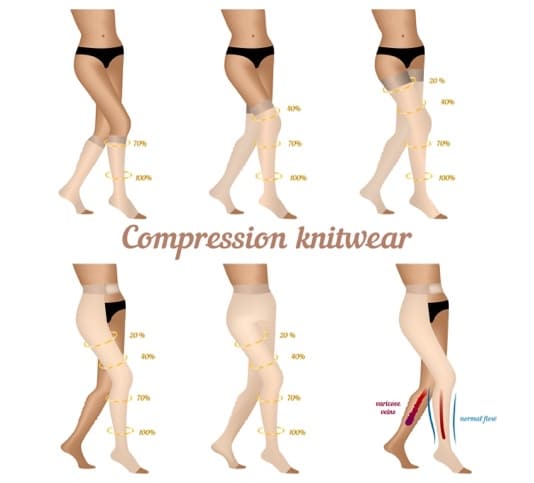
..- The use of properly fitted Graduated Compression Stockings. These stockings exert varying (decreasing) pressures from the ankle upwards, thus decreasing Venous Hypertension and reversing the pooling of blood. (Fig 30, 31)

Fig 30: Graduated Compression Stockings
- AND
- If Venous Insufficiency (VI) is caused by superficial Varicose Veins, Sclerotherapy (Fig 27) is the preventive treatment of choice.
. - When Venous Insufficiency (VI) is caused by incompetent Perforator Veins (Fig 32), Sclerotherapy (Fig 27) is the preventive treatment of choice.
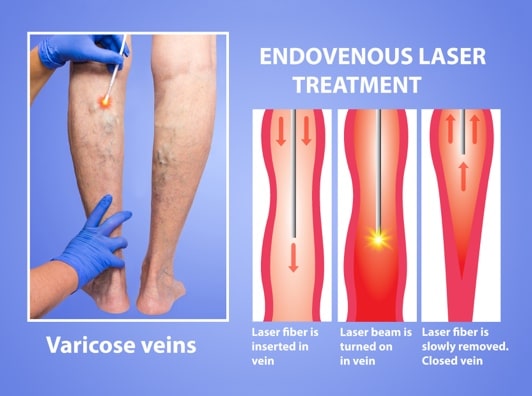
. - If Venous Insufficiency (VI) is caused by Venous Reflux in the Long Saphenous Vein (in old terminology “Great Saphenous Vein”) or in the Short Saphenous Vein (in old terminology “Lesser Saphenous Vein”), the preventative treatment of choice would be Endovenous LASER Treatment (EVLT) (Fig 33) or Radiofrequency (RF) closure (Fig 34).
.
- If Venous Insufficiency (VI) is caused by superficial Varicose Veins, Sclerotherapy (Fig 27) is the preventive treatment of choice.
|
Fig 31: Various models of Graduated Compression Stocking |
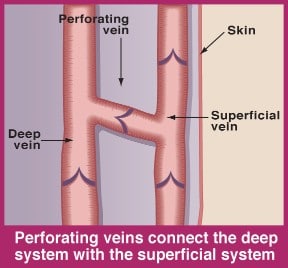
Fig 32: Perforator Veins |
|
Fig 33: Endovenous LASER Treatment |
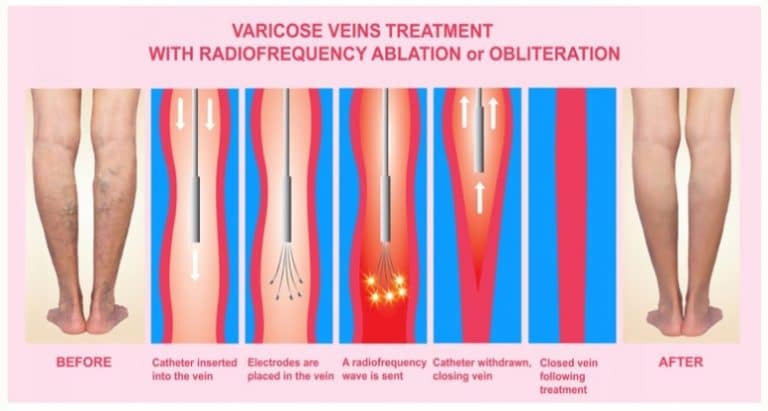
Fig 34: Radiofrequency Closure |
.
- Additional modalities for VLU prevention
.
- In cases that Venous Insufficiency (VI) is caused by Post Thrombotic Syndrome – which is a sequela of prior DVT – your physician may prescribe blood thinners.
. - For female patients who had a VLU in the past or that are judged to be at a high risk for developing VLU, they should avoid the use of contraceptive hormonal medication, Estrogen, and Progesterone products – unless medically indicated by their Obstetrician.
. - Cardiovascular exercise and weight control are encouraged, as they promote healthy blood flow.
. - Heavy lifting and intense bodybuilding exercises are not recommended for patients with Venous Insufficiency (VI)
- In cases that Venous Insufficiency (VI) is caused by Post Thrombotic Syndrome – which is a sequela of prior DVT – your physician may prescribe blood thinners.
-
- Inspection of the patient’s feet on a daily basis by the patient’s spouse or nurse.This is done in order to check if there are any signs of a Wound developing (e.g. blisters, excessive callus, localized swelling or redness, or a small breakage in the skin). It is essential that feet are inspected daily, as patients with Diabetic Neuropathy have impaired sensation and also often times decreased vision – early detection is key.
. - Keeping blood sugar levels under control.
. - Maintaining a healthy weight.
. - Partaking in regular cardiovascular exercises.
. - Using custom-made insoles, or shoes that redistribute the weight evenly over the entire foot (fig 35, 36).
. - Avoiding smoking.
. - Regular nail trimming by a professional podiatrist.
- Inspection of the patient’s feet on a daily basis by the patient’s spouse or nurse.This is done in order to check if there are any signs of a Wound developing (e.g. blisters, excessive callus, localized swelling or redness, or a small breakage in the skin). It is essential that feet are inspected daily, as patients with Diabetic Neuropathy have impaired sensation and also often times decreased vision – early detection is key.
|
Fig 35: Offloading shoe soles |

Fig 36: Custom-made diabetic shoe |
VII. Case Studies
.
View the PowerPoint Presentation (PPT) by Dr. Asad R Shamma at SHAMMA Clinic, Dubai: Treatment of Chronic Wounds
Watch the Live Q&A of Treatment of Chronic Wounds (DFWs) with Dr. Asad R Shamma of SHAMMA Clinic, Dubai
Watch the TV Interview on MBC of Treatment of Chronic Wounds (VLUs) with Dr. Asad R Shamma of SHAMMA Clinic, Dubai
.
VIII. Glossary
.
- ABI: Ankle-brachial pressure index is a simple non-invasive bedside test where the ratio of the blood pressure at the ankle to the blood pressure in the upper arm (brachium) is compared. A low ratio suggests blocked arteries due to peripheral artery disease (PAD).
.
- Arterial Duplex Ultrasound of Legs: (Fig 22) A non-invasive bedside test that uses ultrasound waves and Doppler to examine blood vessels and blood flow in the legs.
.
- Chronic Wound: A barrier (skin in the case of DFW & VLU) defect that has not healed in 3 months.
.
- Compression Bandage (AKA short-stretch bandage if low in elasticity) – (Fig 25): a tubular bandage applied from foot to knee that markedly reduces swelling of the leg without the constriction or the “tourniquet effect” which would otherwise hinder the normal flow of body fluids.
.
- Diabetic Neuropathy: Nerve damage (Fig 9) to peripheral sensory nerves and motor nerves of the legs by Diabetes Mellitus.
. - Decubitus Ulcer (AKA bedsore): (Fig 5) Chronic Wounds localized damage to the skin and/or underlying tissue that usually occur over a bony prominence as a result of pressure in combination with shear and/or friction.
.
- DFW: (Fig 3, 10) A type of Chronic Wound that occurs in 15% of all individuals with diabetes, and recurrence of these ulcers is seen in over 70% of patients. It is caused by PAD (Fig 6) & Neuropathy (Fig 9) acting alone or in combination.
.
- DM (Diabetes Mellitus): A systemic metabolic disease caused by a lack of or a decrease in insulin, or insulin resistance, resulting in high blood-sugar levels. This results in PAD (Fig 6) and Neuropathy (Fig 9) which leads to progressive and irreversible damage to many of the body’s organs (Fig 37).
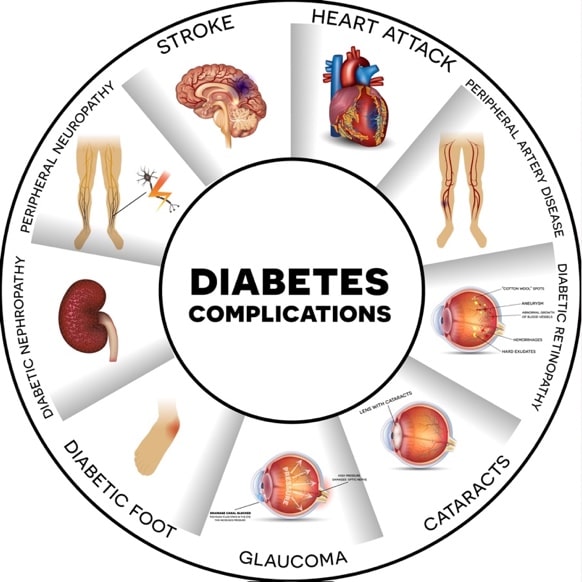
Fig 37: The Spectrum of Diabetes Complications
- Doppler Test: Uses high-frequency sound waves to measure the amount of blood flow in veins and arteries.
.
- DVT (Deep Vein Thrombosis): (Fig 8) A serious medical condition where a blood clot develops in a deep vein, most often in the lower extremity, and results in obstruction of the return of blood to the lungs. A DVT can break loose and migrate to the lung, causing a serious problem called a pulmonary embolism.
.
- Etiology: The cause or manner of causation of a medical condition or disease.
.
- Gaitor Area: The area extending from just above the bony prominences of the ankle (malleoli) to below the knee, where 95% of VLUs occur.
.
- Graduated Compression Stockings: (Fig 30, 31) specially woven, snug-fitting, stretchy socks that gently squeeze the leg and fight Venous Reflux. They are tighter around the ankle and get looser as they move up your leg.
.
- Lateral Malleolus:The prominent bone on the lateral side (outside) of the ankle.
.
- Long Saphenous Vein (Previously known as the greater saphenous vein): A large subcutaneous (under the skin) superficial vein of the leg. It is the longest vein in the body, and runs along the entire length of the lower limb; returning blood from the foot, leg, and thigh to the deep femoral vein in the groin, which drains into pelvic veins, and ultimately the unoxygenated blood returns to the lung.
.
- Lipodermatosclerosis: (Fig 15, 17) Skin changes of the lower legs that occur in patients who have venous insufficiency. It is a type of inflammation of subcutaneous fat that results in hardening and inelasticity of the overlying skin and brownish discoloration. This is referred to as “brawny induration.” (Fig 16) The skin becomes brittle and ulcerates (breaks down) easily when the leg swells, which how a Chronic Wound.
. - Medial Malleolus: The prominent bone on the medial side (inside) of the ankle.
.
- Metatarsal Bone: One of five long bones in the foot that are located between the heel and the toes. (Fig 38).
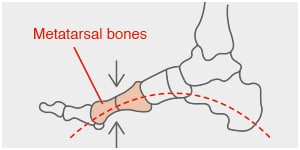
Fig 38: The Metatarsal Bones
- Metatarsal Head: The most prominent and enlarged part of a Metatarsal Bone that is closed to a toe.
.
- Metatarsal Neurotrophic Wound: (Fig 3, 10) A wound that is located over a Metatarsal Head.
.
- Motor Nerve:A nerve that controls muscle action.
.
- Neuropathy: (Fig 9) Damage to the nerves that carry messages to and from the brain and spinal cord. In this article, it refers to nerves of the legs and feet. The Pathophysiology is damage to the outer coating of the nerves called myelin.
.
- Offloading: (Fig 28, 29) A therapeutic strategy of treatment in diabetic foot ulcers, aiming at redistributing the pressure away from an area (typically the sole of the foot or heel that has excessive sustained pressure). It aims to relief these sites of injury.
.
- PAD: (Fig 6) A manifestation of atherosclerosis (hardening of arteries) . PAD is caused by cholesterol plaque buildup leading to blockages or narrowing in the arteries and resulting in decreased blood flow to the affected leg and foot.
.
- Pathophysiology:The mechanism of disorder in a physiological process that leads to a disease or medical condition.
. - Perforator Veins: (Fig 32) Important veins that connect the Long Saphenous Vein and Short Saphenous Vein of the legs to the deep veins of the lower extremity.
- Post Thrombotic Syndrome: Constellation of signs and symptoms that are a result of a DVT (Fig 8)
.
- PPT: PowerPoint Presentation; A Microsoft program that allows the presentation of information in a sequential slide format.
.
- Pressure Wound/Ulcer: Ulcers that occur over bony prominence owing to sustained pressure and/or friction forces that obstruct blood flow to the tissue.
.
- Sclerotherapy: (Fig 27) The treatment of veins by the injection of a medication with the goal of closing the treated vein.
.
- Sensory Nerve: A nerve that carries signals of sensation (e.g. pain and touch) to the brain.
.
- Short Saphenous Vein (Previously known as Lesser Saphenous Veins): The counterpart of the Long Saphenous Vein that runs on the back of the leg (calf) from the ankle to the knee.
.
- Ulcer:A wound that is caused by internal ethology/disease, and is usually chronic. Acute Wounds, on the other hand, are caused by violence, surgical intervention, or are self-inflicted.
.
- Venous Duplex Ultrasound of the Legs: (Fig 22) A non-invasive painless bedside test. Using sound waves and Doppler, your physician can determine if your deep veins are healthy and have unidirectional normal flow of blood or an abnormality. Abnormalities can be either Venous Reflux (Fig 12,13) (bidirectional flow) or obstruction in a vein. Either one of these abnormal findings lead to what is called Venous Insufficiency (VI).
.
- Venous Hypertension:Elevated pressure in a vein, often as result of Venous Reflux or obstruction to the return of venous blood, often caused by DVT (Fig 8)
.
- Venous Insufficiency (VI): (Fig 12, 13, 14, 16) A medical condition that occurs when forward flow through the veins is obstructed or slowed, such as in the case of a DVT (Fig 8), or when there is Venous Reflux (Fig 12, 13).
.
- Venous Stasis Dermatitis (also referred to as venous eczema or stasis dermatitis): A consequence of a prolonged period of Venous Reflux (Fig 12, 13) With blood pooling in the lower part of the leg, fluid and pressure build, and some of the blood leaks out of the veins and into the skin, damaging it.
.
- Venous Reflux: (Fig 12) The abnormal backing up of blood into the vein resulting in pooling of blood in the lower leg. Healthy veins bring blood back to the lung and heart by allowing the blood to flow up the legs. Venous blood is “pumped” primarily by the action of the calf muscles against gravity. To accomplish this, veins have multiple one-way valves with flaps or cusps (in the case of the Long Saphenous Vein, there is an average of 7-9) which act as one-way doors. When the valves do not work properly due to damage from a prior DVT (Fig 8), or much more often genetically inherited weakness in them; the blood does not flow properly upward when we stand, sit, or strain – resulting in pooling of blood in the lowermost part of our lower extremity.
.
- VLU:(Fig 2) A leg ulcer caused by sustained levels of Venous Hypertension in the lower leg due to inadequate venous return.
.
- Varicose Veins (VV): (Fig 12, 13, 14) Enlarged, abnormal, tortuous, and protruding abnormal veins that are easily visible on the legs when a person stands or strains.
.
- Wound: A full-thickness skin or barrier defect.
.
- Wound Debridement: (Fig 26) The act of removal of slime and dead tissue from Chronic Wounds with the aim of stimulating the healing process.


 العربية
العربية 










 Get Directions
Get Directions


